Executive Summary
Perimenopause marks a crucial transition period in a woman’s life, beginning typically in her 40s and lasting several years. This phase often brings physical, emotional, and mental challenges due to the natural fluctuation of hormones like estrogen and progesterone. Symptoms such as hot flashes, anhedonia, weight gain, itchy skin, pelvic floor weakness, night sweats, mood swings, sleep disturbances, and cognitive changes affect millions of women globally, often disrupting daily life and well-being.
As many women (including myself) seek alternatives to traditional treatments, cannabis has emerged as a compelling option, gaining interest due to its range of potential benefits. Various components in cannabis, especially cannabidiol (CBD) and tetrahydrocannabinol (THC), interact with the body’s endocannabinoid system (ECS), which plays a role in regulating mood, sleep, pain, and more. As research advances, anecdotal and emerging scientific evidence indicate that cannabis may provide symptom relief for women in perimenopause, supporting an enhanced quality of life we all deserve.
This paper explores the benefits and limitations of cannabis use during perimenopause, specifically focusing on symptom relief, the physiological mechanisms involved, and the current scientific understanding of its role in women’s health during this critical life stage.
1. Introduction to Perimenopause
Perimenopause is the transitional period leading up to menopause, sometimes called the “second puberty”, where ovarian function gradually declines, affecting the levels of estrogen and progesterone. While every woman’s experience is unique, common symptoms include:
• Vasomotor Symptoms: Hot flashes, night sweats
• Mood Disturbances: Anxiety, irritability, mood swings
• Sleep Disruptions: Difficulty falling or staying asleep
• Cognitive Symptoms: “Brain fog,” memory lapses, anhedonia
• Physical Changes: Joint pain, reduced libido, weight gain
The conventional approach to managing these symptoms often includes hormone replacement therapy (HRT), antidepressants, and lifestyle modifications. However, these options may not be effective or suitable for all women, leading many to explore alternative therapies. Cannabis, with its potential anti-inflammatory, analgesic, and anxiolytic properties, presents a promising avenue for relief. Additionally, the cannabinoids in cannabis are estrogenic meaning they work more effectively when estrogen is present, cannabis is quite literally made for women.
2. The Science of Cannabis and the Endocannabinoid System (ECS)
Cannabis contains over 100 cannabinoids, including THC (tetrahydrocannabinol) and CBD (cannabidiol). Both interact with the endocannabinoid system (ECS), a complex network of receptors and neurotransmitters spread throughout the body and brain that regulates critical functions like mood, pain perception, immune response, and sleep.
• THC: Known for its psychoactive effects, THC binds primarily to CB1 receptors in the brain, helping to modulate pain, mood, and appetite.
• CBD: Non-psychoactive, CBD interacts indirectly with CB1 and CB2 receptors, with potential to reduce inflammation, anxiety, and stress responses.
The ECS is closely involved in many areas affected by perimenopausal symptoms, providing a rationale for why cannabis compounds might alleviate some of these challenges. Studies suggest that as estrogen levels drop, the ECS may become less efficient, potentially contributing to symptoms like mood swings, insomnia, and joint pain. Thus, supplementing with cannabinoids may help support the ECS and mitigate some perimenopausal symptoms.
3. Cannabis for Perimenopausal Symptom Relief
3.1 Relief from Hot Flashes and Night Sweats
Hot flashes and night sweats are among the most common and disruptive perimenopausal symptoms. The cause of these symptoms is linked to changes in the hypothalamus, which regulates body temperature, due to fluctuating estrogen levels.
While specific research on cannabis and hot flashes is limited, anecdotal evidence suggests that certain cannabis strains or formulations (particularly those with a balanced CBD:THC ratio) may help in temperature regulation and offer relief. Some women report that cannabis oil or edibles taken before bed helps to reduce night sweats, which can, in turn, improve sleep quality.
3.2 Sleep Improvement
Sleep disturbances affect nearly 40-60% of women in perimenopause, often exacerbated by night sweats, anxiety, and hormonal shifts. A well-functioning ECS promotes better sleep by maintaining homeostasis, and cannabinoids, especially CBD, may support this process.
CBD is known to have calming effects without the “high” associated with THC, which makes it ideal for promoting relaxation before bed. Additionally, THC has been shown to reduce the time it takes to fall asleep. However, higher doses of THC may reduce REM sleep, which can impact dream cycles and sleep quality. A tailored approach, combining low THC with higher CBD, may work best for women looking for sleep support.
3.3 Anxiety and Mood Stability
Hormonal shifts during perimenopause can have a profound impact on mood, leading to symptoms like irritability, anxiety, and even depression. Cannabinoids may help stabilize mood through the ECS. Both THC and CBD have been studied for their anxiolytic and antidepressant effects, potentially helping women to manage stress and anxiety.
• CBD: Known for its anxiolytic properties, CBD may reduce feelings of anxiety and promote calmness without causing a mindshift.
• THC: At lower doses, THC aids in relaxation, but higher doses may increase anxiety in some people. Microdosing—consuming very low doses of THC typically under 5mgs —might help alleviate mood symptoms without strong psychoactive effects.
3.4 Pain and Inflammation Management
Joint pain and muscle aches are common complaints during perimenopause, often stemming from estrogen decline, which affects collagen production and joint lubrication. Cannabis, particularly CBD, is well-regarded for its anti-inflammatory properties, which may reduce pain and stiffness.
Studies have shown that both CBD and THC have potential analgesic effects, and their anti-inflammatory properties may help reduce symptoms of joint and muscle pain. Topical CBD products are increasingly popular among women seeking localized pain relief, offering targeted action without systemic effects. Topicals formulated with moisturizer will also help alleviate dry, itchy skin sometimes associated with perimenopause.
3.5 Cognitive Clarity and “Brain Fog” Relief
Many women experience cognitive challenges during perimenopause, including memory lapses and difficulty concentrating, often termed “brain fog.” While more research is needed, cannabinoids may potentially help improve focus and clarity, especially CBD, which does not impair cognition.
Some preliminary studies suggest that CBD may have neuroprotective properties, possibly supporting brain health and reducing inflammation, which can contribute to improved cognitive function. The right cannabis strain or ratio might help manage brain fog, allowing women to feel more mentally sharp during this transition.
4. Methods of Cannabis Consumption for Perimenopausal Symptom Relief
Women interested in exploring cannabis for perimenopausal symptom relief have several options, including:
• Inhalation (Smoking or Vaping): Provides quick relief but may not be suitable for women with respiratory concerns. Vaporization doesn’t involve combustion of plant matter, making it a more gentle option on the lungs.
• Edibles: Offer longer-lasting effects, ideal for sleep support, though onset time can vary and keep in mind some people’s kidneys do not process edibles through efficiently to make them psychoactive.
• Drinkables: liquid cannabis infusions metabolize in the body more like a smokers high, meaning it will take effect quickly, but will also dissipate fairly quickly as well. An excellent entry point for new users.
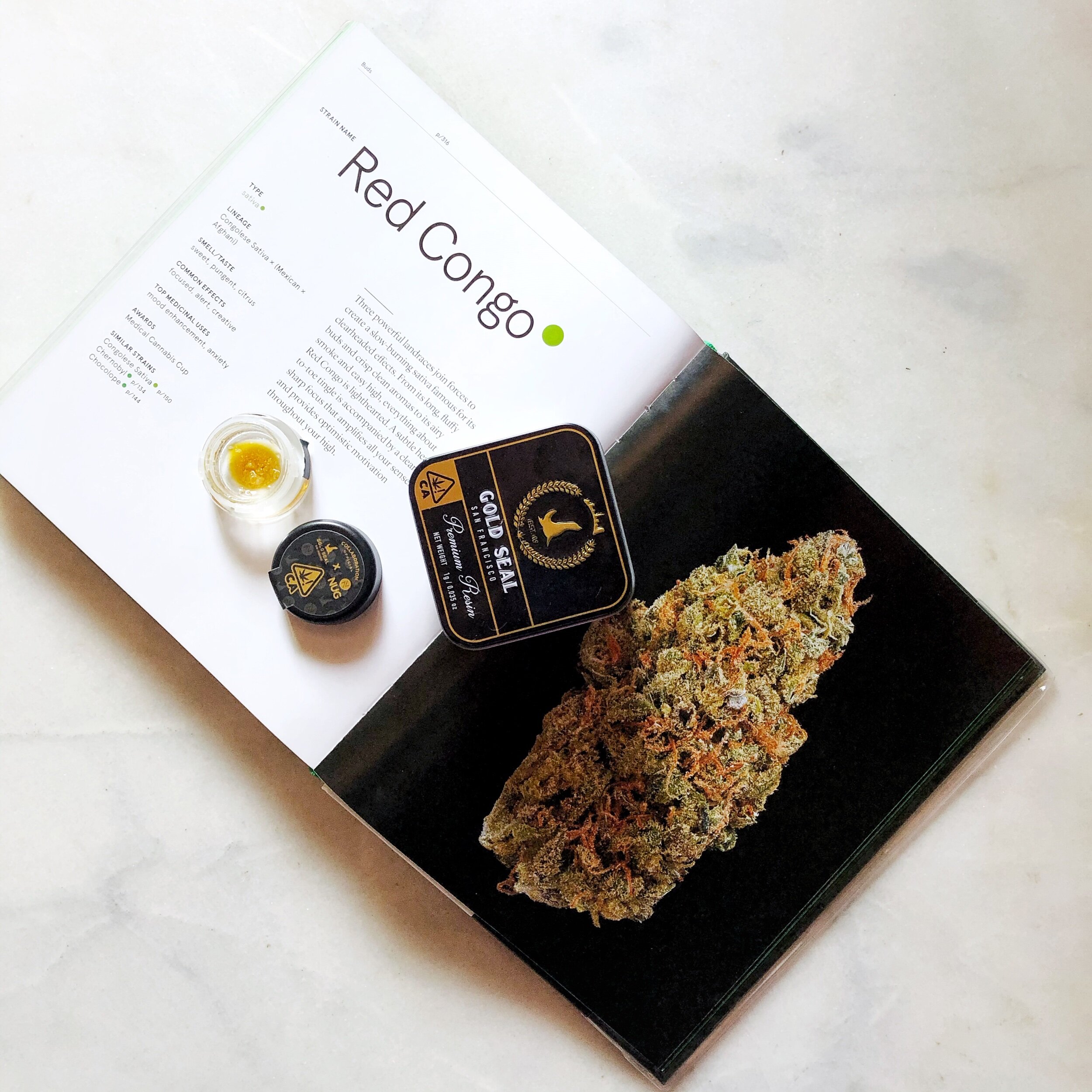
• Tinctures, extracts and Oils: Provide flexible dosing and quicker onset than edibles, with the advantage of precise dosage control. These products are formulated to be taken under the tongue (‘sublingual’) or between the gums and cheek, which is called ‘buccal dosing’. these go directly to the circulatory system, bypassing the digestive system, making it take affect more quickly.
• Topicals: Ideal for localized pain, allowing direct application to sore areas with minimal (if any) psychoactive effects. There are also transdermal patches impregnated with cannabis in various forms, many that do not produce a mind shift but do confer extended release pain relief.
Each method offers unique benefits and onset times, so individual preferences and specific symptoms should guide the choice of consumption.
5. Potential Risks and Considerations
While cannabis is generally considered very safe, it is essential for women to consult with a an expert as well as their healthcare provider (these are often not the same person), particularly because psychoactive effects of THC may have potential for interactions with medications like heart meds or anti-psychotics (cannabis can alter the efficacy of certain medications).
Potential side effects include:
• Psychoactive Effects: THC can cause euphoria that borders on disorientation in higher doses. Microdosing and using a combination of cannabinoids simultaneously minimizes these effects.
• Interaction with Hormone Therapy: Women using HRT should discuss cannabis use with their doctor to avoid any potential interactions (or just to let them know). Again, cannabinoids are estrogenic meaning they work very well when estrogen is present.
• Individual Variation: Each woman’s body responds differently to cannabinoids, and factors like metabolism, hormone levels, mindset, fitness, and ECS sensitivity (aka tolerance) can influence efficacy and side effects.
6. Conclusion: A Personalized Path to Well-Being
Cannabis shows extreme promise in addressing several perimenopausal symptoms, from sleep disturbances and mood swings to joint pain and anxiety. However, every woman’s experience with cannabis is unique, and it may take some experimentation with dosages, strains, and delivery methods to find the right fit. Using cannabis as medicine is incredibly personal and the good news is that in today’s product landscape, there are products available for consumers to ingest just 1 mg at a time making cannabis a very friendly option for new users.
For women seeking natural, plant-based alternatives, cannabis provides a customizable option for managing the symptoms of perimenopause. As research progresses and awareness grows, cannabis will absolutely become a more widely accepted and understood tool in the perimenopausal journey.
If you or a loved one would like personalized guidance on your cannabis journey you can schedule time on my calendar for a confidential consult here.